The Best and Worst Reasons to Induce Labor
Although few true reasons to induce labor exist, labor induction is rapidly becoming routine procedure despite mounting research evidence that inductions are twice as likely to end in cesarean section and put the baby at twice the risk of experiencing fetal distress. At present, 1 in 5 labors are induced, more than twice the recommended level.
OVERDUE PREGNANCY
One of the most commonly-cited reasons for induction is an overdue pregnancy. However, this is an arbitrary statement, especially as the average gestation of a first-time pregnancy worldwide is 41 weeks, 1 day. In the US, however, for many doctors it is routine procedure to induce labor by 40 weeks, despite research evidence showing women can safely carry to 42 weeks in low-risk pregnancies. It is still unknown what combination of factors causes labor to spontaneously begin. It can be initiatied through various medical ways to induce labor or by other natural ways to induce labor, but not in the same manner in which spontaneous labor begins.
The American Congress of Obstetricians and Gynecologists (ACOG) now recommends elective induced labor should not occur before 39 weeks gestation in response to current research evidence showing decreased fetal outcomes in induced labors and doubled risks of cesarean section.
Another variable is the accuracy of the due date itself. Due dates are typically calculated from the first day of the woman's last period (LMP). However, this method is only accurate for women who have a regular 28-day cycle and ovulate on day 14. For women with long and/or irregular cycles or those who ovulate early/late, the calculated due date can be weeks off in either direction.
A reliable estimate of the due date can be obtained via a transvaginal ultrasound between 8-10 weeks gestation which carries a maximum standard error of measure of +/- 3 days. It's important to note that as pregnancy progresses, ultrasound becomes a less reliable measure. In the advanced stages of pregnancy, the standard error of measure of an ultrasound varies by +/- 2 weeks and fetal weight estimates can be off by as much as 2 pounds in either direction. For this reason, a single late-term ultrasound should never be used as one of the reasons to induce labor, to change a due date, or to predict a baby is too large to negotiate the mother's pelvis.
THE BABY IS TOO BIG
While this is commonly cited as one of the reasons to induce labor, there is little research evidence to support the claim. Induction is commonly scheduled when fetal weight is thought to be macrosomic or large for gestational age. Fetal macrosomia is defined as either birth weight of 4000-4500 g (8lb 13oz-9lb 15oz) or greater than 90% for gestational age based on gender and ethnicity. Macrosomia affects 1-10% of all pregnancies.
However, a diagnosis of fetal macrosomia can only be confirmed after birth; therefore, the condition cannot definitively be diagnosed during pregnancy.
The true issue lies in that fetal weight alone is not a reliable indicator of which babies will have difficulty being born. Many factors affect how well a baby will negotiate the mother's pelvis, including head circumference, body positioning, abdominal circumference, and fetal presentation in addition to the mother's freedom of movement and choice of birth positions during labor. Cephalopelvic disproportion, which indicates a baby too large for the pelvic outlet, cannot be diagnosed by fetal weight alone. Separate studies by Gonen et al, Leaphart et alt, Friesen et alt, and Combs et alt all support that induction at term is not recommended to avoid birth trauma for suspected large babies. It was found to increase the c-section rate and associated problems for mother and baby, but did not reduce the shoulder dystocia rate, nor improve birth outcomes.
Tired of Being Pregnant
While the later days of pregnancy can be uncomfortable, induction is not the answer. This time is but the smallest span and will pass once the baby arrives in its own time. Once a mother holds her baby for the first time, all the woes of pregnancy will be forgotten.
In other cases, a family may elect to schedule an induction because it's convenient: out-of-town family will be there, the preferred medical provider is available, etc. Seldom are these true reasons to induce labor. Sometimes making the responsible choice is inconvenient. Do it anyway.
While the above represents a sampling of the worst reasons to induce labor, below are circumstances which indicate an induction may be truly medically necessary.
PRE-EXISTING MATERNAL HEALTH CONDITIONS
If the mother has health problems such as heart disease, seizure disorder, hypertension, cancer or any other serious medical conditions, induction may be indicated. However, many women with some of these conditions give birth naturally. Each case should be considered on an individual basis after an open discussion of all potential options with the care provider.
PRE-EXISTING BABY HEALTH CONDITIONS
In some cases, a family may know their baby has a congenital condition which requires intervention or special care at birth. In these circumstance, the controlled environment of an induction may be one of the valid reasons to induce labor.
Circumstances that prohibit an induction
The following situations prohibit an induction, and some may require a scheduled cesarean section:
- Placenta previa (when the placenta lies over the cervix) or vasa previa (when blood vessels from the umbilical cord are embedded in the amniotic membranes and are at risk for rupture during labor)
- When the cord is lying in front of the baby's head and could be compressed as the head enters the birth path or prolapse through the cervix when the membranes rupture.
- A prior c-section.
- A previous c-section with a "classical" (vertical) uterine incision or other uterine surgery, such as a myomectomy (surgery to remove fibroids).
- Expecting higher-order multiples, i.e. triplets or more.
- An active genital herpes infection.
Determining Readiness for Induction
As addressed previously, no method of induction is guaranteed to be successful if the cervix is not ripe. This can often be a factor in an induction that turns into a failure-to-progress c-section. A guide that is commonly used to determine the potential success of an induction is the Bishop's score.
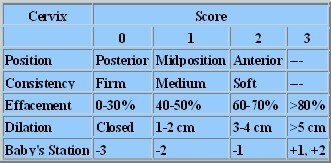
The term Bishop's Score refers to a group of
measurements used to determine whether a woman's cervix is ripe for induction. The Bishop's score
alone should never be used as one of the reasons to induce labor. The Bishop's Score is based on the
baby's station (location in the mother's pelvis), dilation, effacement, position and consistency. A
score from 7-10 is most desirable when considering induction.
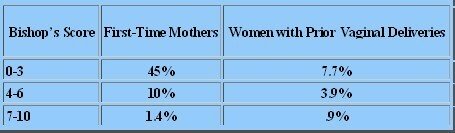
The following chart illustrates the percentage of cesarean sections after failed induction as related to the Bishop score.
Here is a chart to help calculate the Bishop's score. A high Bishop's score in itself is not one of the reasons to induce labor. It does not mean an induction is needed. It is simply a measure of whether or not the labor induction is likely to be successful.
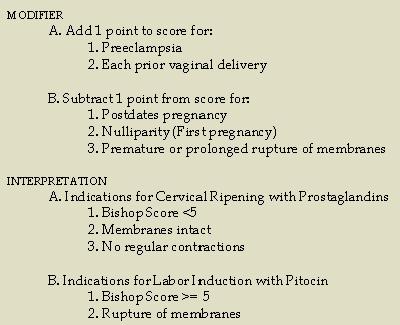
If the Bishop's Score is below a 7, the mother is less than 41 weeks and is not experiencing any health conditions, then induction is likely not warranted. Make informed decisions when assessing the reasons to induce labor for both the mother and baby's well-being.
References
G¸lmezoglu AM, Crowther CA, Middleton P. Induction of labour for improving birth outcomes for women at or beyond term. Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No.: CD004945. DOI: 10.1002/14651858.CD004945.pub2.Combs CA, Singh NB, Khoury JC. Elective induction versus spontaneous labor after sonographic diagnosis of fetal macrosomia. Obstet Gynecol. Apr 1993;81(4):492-6.
Coomarasamy A, Connock J, Thornton J, Khan KS. Accuracy of ultrasound biometry in the prediction of macrosomia: a systematic quantitative review. BJOG. 2005;112:1461-66.
De Reu PA, Smits LJ, Oosterbaan HP, Nijhuis JG. Value of a single early third trimester fetal biometry for the prediction of birth weight deviations in a low risk population. J Perinat Med. 2008;36(4):324-9.
Dodd JM, Crowther CA. Elective repeat caesarean section versus induction of labour for women with a previous caesarean birth. Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No.: CD004906. DOI: 10.1002/14651858.CD004906.pub2.
Friesen CD; Miller AM; Rayburn WF. Influence of spontaneous or induced labor on delivering the macrosomic fetus. Am J Perinatol 1995 Jan;12(1):63-6.
Gonen O, Rosen DJ, Dolfin Z, et al. Induction of labor versus expectant management in macrosomia: a randomized study. Obstet Gynecol. Jun 1997;89(6):913-7.
Harman & Kim. "Current Trends in Cervical Ripening and Labor Induction" American Family Physician 1999; 60:477-84.
Hackmon R, Bornstein E, Ferber A, Horani J, O'Reilly Green CP, Divon MY. Combined analysis with amniotic fluid index and estimated fetal weight for prediction of severe macrosomia at birth. Am J Obstet Gynecol. Apr 2007;196(4):333.e1-4.
Irion O, Boulvain M. Induction of labour for suspected fetal macrosomia. Cochrane Database of Systematic Reviews 1998, Issue 2. Art. No.: CD000938. DOI: 10.1002/14651858.CD000938.
Leaphart WL; Meyer MC; Capeless EL. Labor induction with a prenatal diagnosis of fetal macrosomia. J Matern Fetal Med 1997 Mar-Apr;6(2):99-102.
Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Kirmeyer S. Births: final data for 2004. Natl Vital Stat Rep. Sep 29 2006;55(1):1-101.
Mondestin MA, Ananth CV, Smulian JC, Vintzileos AM. Birth weight and fetal death in the United States: the effect of maternal diabetes during pregnancy. Am J Obstet Gynecol. Oct 2002;187(4):922-6.
Mulik V, Usha Kiran TS, Bethal J, Bhal PS. The outcome of macrosomic fetuses in a low risk primigravid population. Int J Gynaecol Obstet. Jan 2003;80(1):15-22.
Return from Reasons to Induce Labor to Natural Ways to Induce Labor
Return to Giving Birth Naturally Home
Page Last Modified by Catherine Beier, MS, CBE
Most Popular
How to Use Acupressure to Induce Labor
Childbirth Relaxation Script MP3s
Nutrition During Pregnancy - Nix the Notion of Eating for Two
Looking for a Birth Professional? Search our Provider Directory
Online Childbirth Classes
Choose 7 week, 12 week, or Self- Paced online childbirth classes available wherever and whenever you need them.
Featured Birth Story
Vanessa's natural birth story shows that when birth is left alone to proceed as it should, it waits for no one - not even doctors or midwives.
Free Pregnancy Tickers
Create a free pregnancy ticker to post on your blog, website, Facebook profile or favorite social media...